Health workers treating patients with the coronavirus may be at the top of the line to get a vaccine once one is approved. But that’s not necessarily the obvious move.
The National Vaccine Advisory Committee met Wednesday for the first of a two-day public meeting on the Covid-19 pandemic, vaccine developments and a distribution plan whenever one is ready.
“The question is, how at risk are healthcare workers, especially in the United States, especially in the era of adequate PPE,” Dr. Ezekiel Emanuel, chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania, said at the meeting. ”Because at least in our hospital, transmission from patient to doctor with PPE [is] zero.”
The National Academies of Sciences, Engineering, and Medicine released a draft proposal for U.S. distribution U.S. earlier this month that prioritizes health-care workers and vulnerable Americans, such as the elderly and those with underlying health conditions. The group formed the draft proposal at the request of the Centers for Disease Control and Prevention, which estimates that there are between 17 million and 20 million health-care workers in the U.S.
“Front-line health care workers are particularly important in stemming the pandemic and preventing death and severe illness,” the group wrote in a section of the report titled “Rationale.” “From the beginning of the pandemic, many frontline workers have worked in environments where they have been exposed to the virus, often without adequate PPE.”PPE refers to personal protective equipment, such as masks, gloves and gowns that are used to prevent the spread of infectious diseases.
Reports continue to emerge across the country of health-care workers suffering from shortages of crucial PPE, which have plagued the U.S. response to the pandemic since the beginning. PPE refers to personal protective equipment, such as masks, gloves and gowns that are used to prevent the spread of infectious diseases.
Emanuel added that the prioritization of a potentially life-saving vaccine is “very, very complex” and noted that the placement of all health-care workers in the first group for prioritization is “probably not justified at this point in the course of the pandemic.”
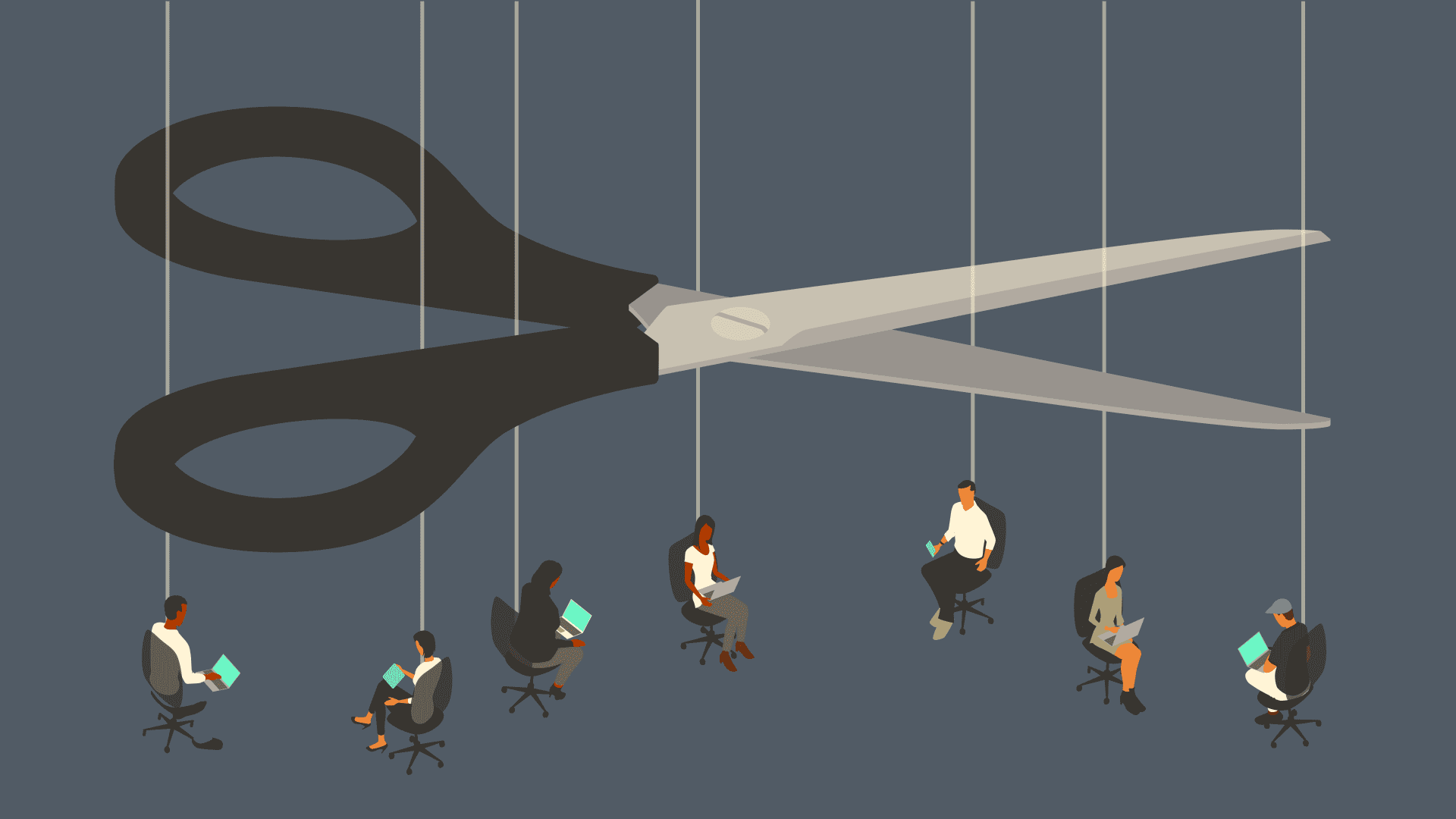
The panel presenting to NVAC set out a potential framework for thinking through the tricky ethical issues of how vaccines should be distributed. Vaccines won’t be available to the entire population at once, so certain populations will likely need to be prioritized over others.
So should health workers in the United States be vaccinated first, potentially ahead of essential workers at meat packing plants, schools, or at grocery stores? The elderly in nursing homes are another group that bio-ethicists would prioritize, given the high rates of mortality for those that contract the virus.
Emanuel noted that at this stage in the pandemic, many of the medical workers at his hospital — and at other health systems — now have access to sufficient PPE, thereby reducing their risk of contracting the virus. More consideration is needed, however, to better determine exactly which workers within a hospital are most at-risk for infection, he said.
“What high-risk job should get first priority,” he asked. “How many of you think firemen are really at high risk, or are we just lumping them in? So it seems to me we do need a serious determination of risk here if that’s our justification.”
Dr. Emanuel pointed to the importance of modeling out the potential risk, before jumping to conclusions.
Others in the panel noted that health workers may still be at high-risk because not everyone has access to PPE. That might include home health workers, nursing aides, hospital security or staff delivering food to sick patients.
Dr. Sara Oliver, an epidemic intelligence service officer with CDC’s Division of Viral Diseases, acknowledged that having appropriate PPE has reduced the spread of the coronavirus in health-care settings. However, she noted that the front-line medical workers who are most at-risk for infection are often not the doctors and nurses, but instead the security personnel, nursing aides, deliver workers and others who might not have access to PPE.
“While we should do everything we can to make sure that people who need PPE get it, I don’t know that it completely removes the importance of health-care workers being protected early,” she said Wednesday at the meeting.
The panel also discussed that many front-line medical personnel might be experiencing “PPE fatigue,” which could place workers in health-care settings at greater risk.
Emanuel noted that if certain health workers are more at-risk than others, then the distribution plan should specifically prioritize those at-risk groups. But he added that grouping them all together “does not seem to me to be the justifiable approach.”
“The goal is to reduce harm and maximize benefit. You have to look at how much vaccine is going to do how much good in one group,” Emanuel said.
He added that the question of who to prioritize may very well depend on which vaccine is authorized and what the trial data says about the immunization. He said that if a vaccine reduces transmission of the virus but doesn’t reduce the severity of the disease, or vice versa, it could have distribution implications.